By 2025, superbugs are rising due to widespread antibiotic misuse, which lets bacteria quickly evolve resistance. Overprescription, skipping doses, and self-medicating worsen the problem, making infections harder to treat and increasing healthcare struggles. Hospitals also see more resistant bacteria spreading, risking patient health and raising costs. To fight back, stricter stewardship, better diagnostics, and awareness are vital. Stay with us to discover how we can turn the tide on this growing threat.
Key Takeaways
- Antibiotic misuse and overprescription accelerate bacterial resistance, leading to more superbugs by 2025.
- Enhanced infection control and stewardship programs are vital to slow resistance growth.
- Development of new antibiotics and rapid diagnostics will be crucial in combating resistant bacteria.
- Public awareness campaigns aim to reduce misuse and promote responsible antibiotic use.
- Global collaboration and stricter regulations are essential to address rising superbug threats by 2025.
Have you noticed how infections once easily treated with antibiotics are becoming more resistant? It’s a growing concern that threatens to undo decades of medical progress. The rise of superbugs isn’t just about bacteria evolving; it’s also driven by human actions, particularly antibiotic misuse. When antibiotics are overprescribed or taken incorrectly—like skipping doses or stopping early—bacteria have a chance to adapt and develop resistance. This misuse doesn’t happen only in hospitals; it’s a widespread issue that includes self-medication, incomplete courses, and over-the-counter sales in some regions. As a result, infections that once responded swiftly to antibiotics are now lingering or becoming more severe, complicating treatment plans.
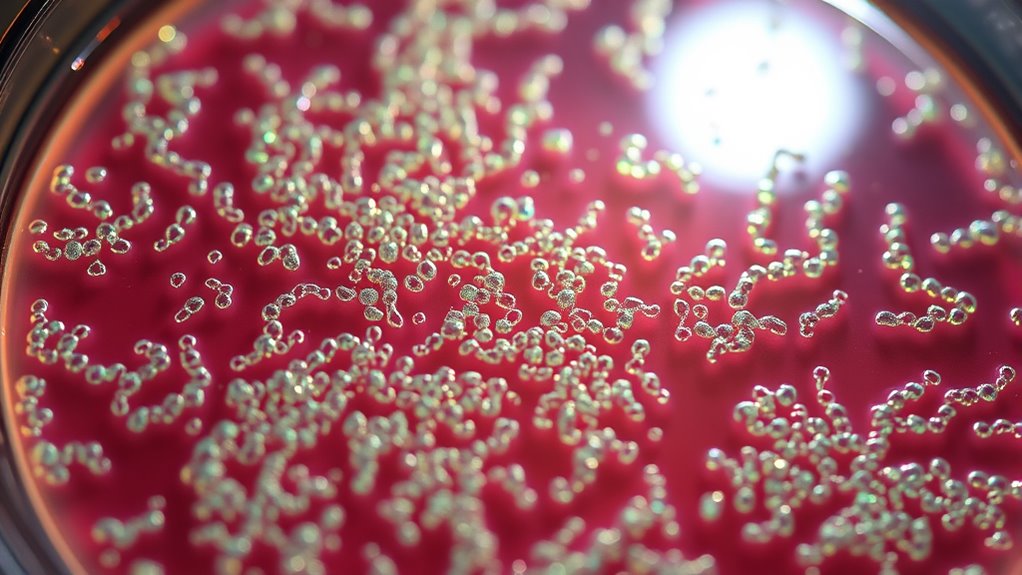
In hospitals, the problem becomes even more urgent. Hospital infections, especially those caused by multidrug-resistant bacteria, have skyrocketed in recent years. These environments are where antibiotics are most frequently used, often as a first response to infections. But when hospitals don’t rigorously follow infection control protocols, resistant bacteria can spread rapidly among vulnerable patients. Devices like catheters, ventilators, and surgical tools can become reservoirs for superbugs if not properly sterilized, turning hospitals into breeding grounds for resistant strains. Patients with weakened immune systems, chronic illnesses, or those undergoing invasive procedures are at heightened risk. Once infected, these patients face longer hospital stays, increased complications, and higher mortality rates.
The rise of hospital infections caused by resistant bacteria is alarming because it reduces the effectiveness of our most potent antibiotics. This, in turn, forces healthcare providers to resort to older, more toxic drugs or experimental treatments that might not be as effective. Meanwhile, the cycle of antibiotic misuse continues, fueling the problem further. It’s a vicious circle—more infections lead to more antibiotic use, which then accelerates resistance. Efforts to curb this trend include stricter antibiotic stewardship programs, better diagnostic tools to ensure appropriate prescriptions, and increased awareness about the dangers of misuse. But without widespread behavioral change, hospitals will remain battlegrounds where superbugs thrive.
Understanding the connection between antibiotic misuse and hospital infections is essential. It’s up to healthcare professionals, patients, and policymakers to work together to reduce unnecessary antibiotic use and improve infection control. Only by doing so can we slow down the rise of superbugs and preserve the effectiveness of antibiotics for future generations. Recognizing the importance of antibiotic stewardship and infection control measures is vital for tackling this crisis. The fight against resistance is complex, but addressing hospital infections and antibiotic misuse is a key step toward winning it.
Frequently Asked Questions
How Quickly Are Superbugs Expected to Spread Globally?
The global spread of superbugs is expected to accelerate rapidly, with transmission speed increasing due to international travel and interconnected healthcare systems. You should stay vigilant, as these resistant bacteria can spread within days or weeks, making containment challenging. Efforts to improve hygiene, responsible antibiotic use, and global cooperation are vital to slow down this transmission speed and prevent widespread infections.
What New Antibiotics Are in Development to Combat Superbugs?
Imagine opening new doors in a fortress—that’s what novel antibiotics aim to do against superbugs. Researchers are developing innovative drugs targeting resistance mechanisms, such as beta-lactamase inhibitors and bacteriophage therapy, to outsmart resistant bacteria. These new antibiotics are designed to pierce defenses and restore effectiveness. By staying ahead of resistance, you help guarantee these powerful tools continue fighting superbugs effectively, safeguarding your health and the future of medicine.
How Can Individuals Reduce Their Risk of Antibiotic-Resistant Infections?
You can reduce your risk of antibiotic-resistant infections by practicing good personal hygiene, like washing your hands regularly and keeping wounds clean. Avoid demanding antibiotics for viral illnesses and always follow your healthcare provider’s advice through proper antibiotic stewardship. Staying vaccinated, staying informed about infections, and maintaining a healthy lifestyle also help prevent infections and reduce the spread of superbugs. These steps protect both you and your community.
What Role Do Agricultural Practices Play in Antibiotic Resistance?
You’re playing with fire if you overlook how agricultural practices impact antibiotic resistance. Antibiotics in farming, especially for livestock, promote resistant bacteria, which can transfer to humans. Excessive crop pesticide use can also upset soil bacteria balance, fostering resistant strains. By supporting sustainable farming and reducing reliance on antibiotics and pesticides, you help slow resistance’s spread. It’s a risk you don’t want to take, so stay informed and advocate for safer practices.
Are There Effective Vaccines Against Resistant Bacterial Strains?
There are emerging vaccines designed to combat resistant bacterial strains, leveraging advances in vaccine development and bacterial immunity. These vaccines aim to boost your immune system’s ability to fight specific superbugs, reducing reliance on antibiotics. While some vaccines are in clinical trials or early deployment, ongoing research continues to improve their effectiveness. Staying updated on these developments helps you understand how immunization can be a key tool against antibiotic-resistant bacteria.
Conclusion
If you don’t act now, these superbugs could take over the world, turning hospitals into battlegrounds and medicine into useless relics. Imagine a future where simple cuts are deadly, and antibiotics vanish like smoke. The fight against resistance isn’t just a battle—it’s a fight for your life’s very fabric. So, stand up, spread awareness, and push for change before these tiny monsters become unstoppable, and the world as you know it crumbles into chaos.